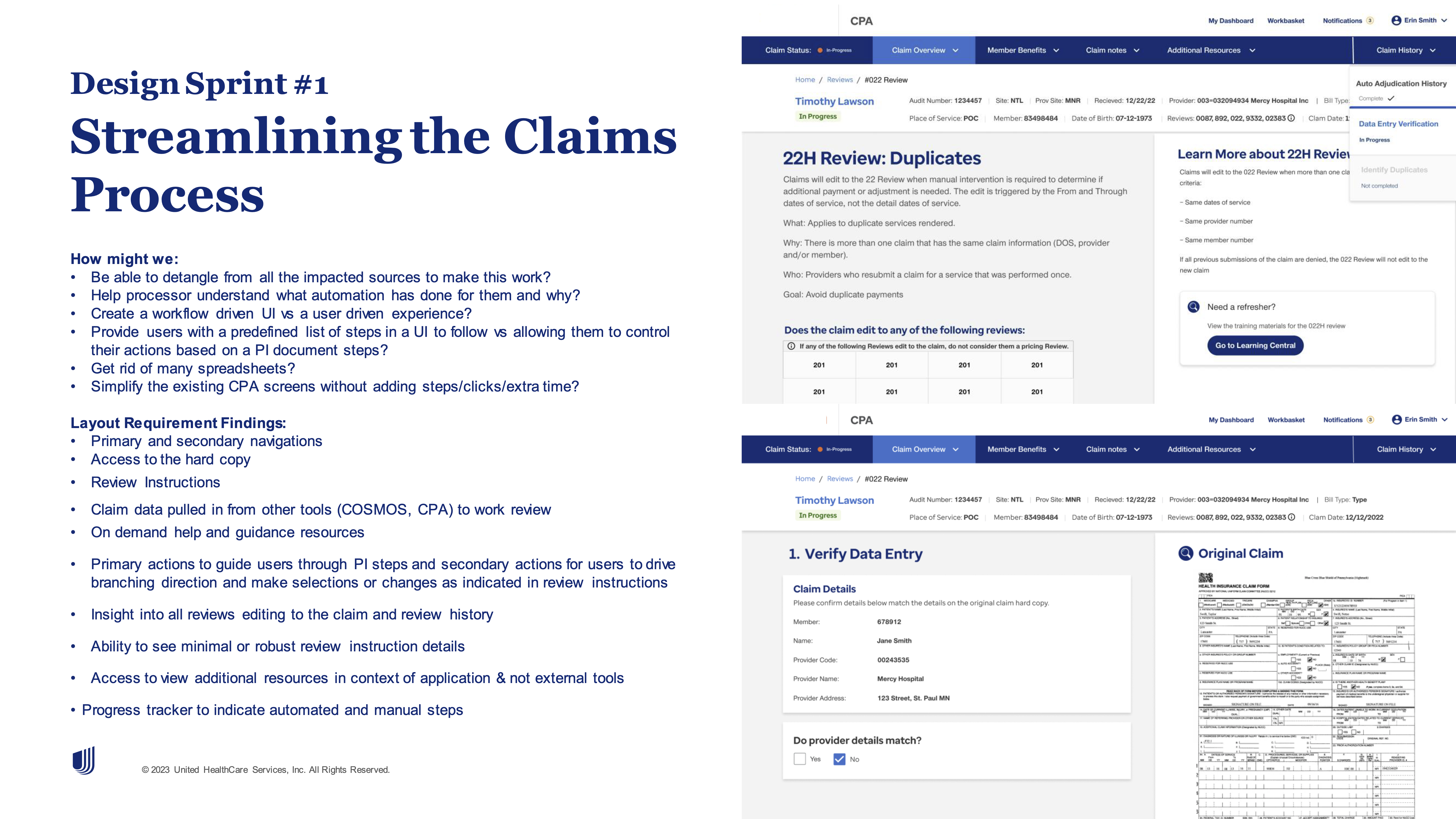
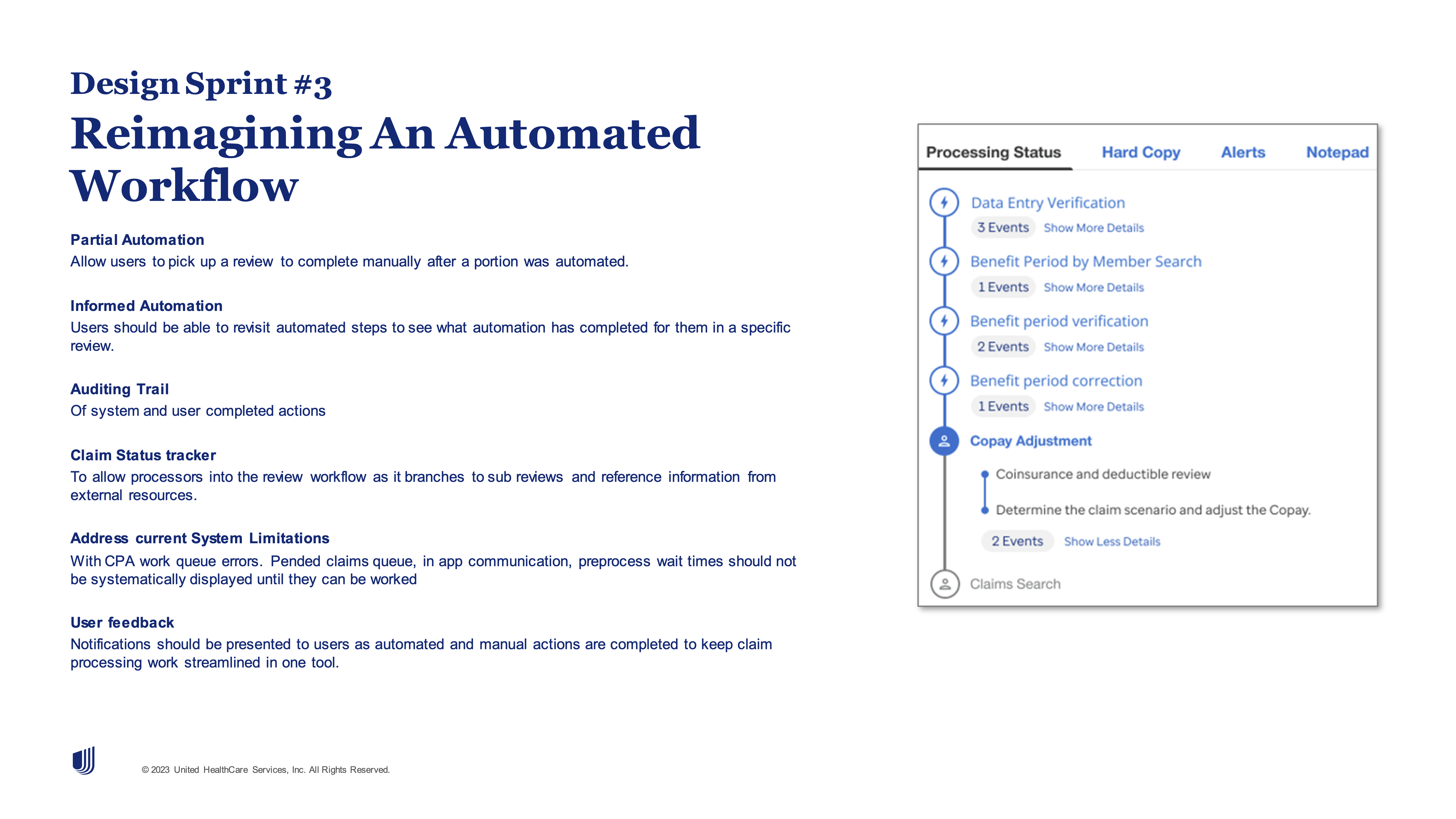
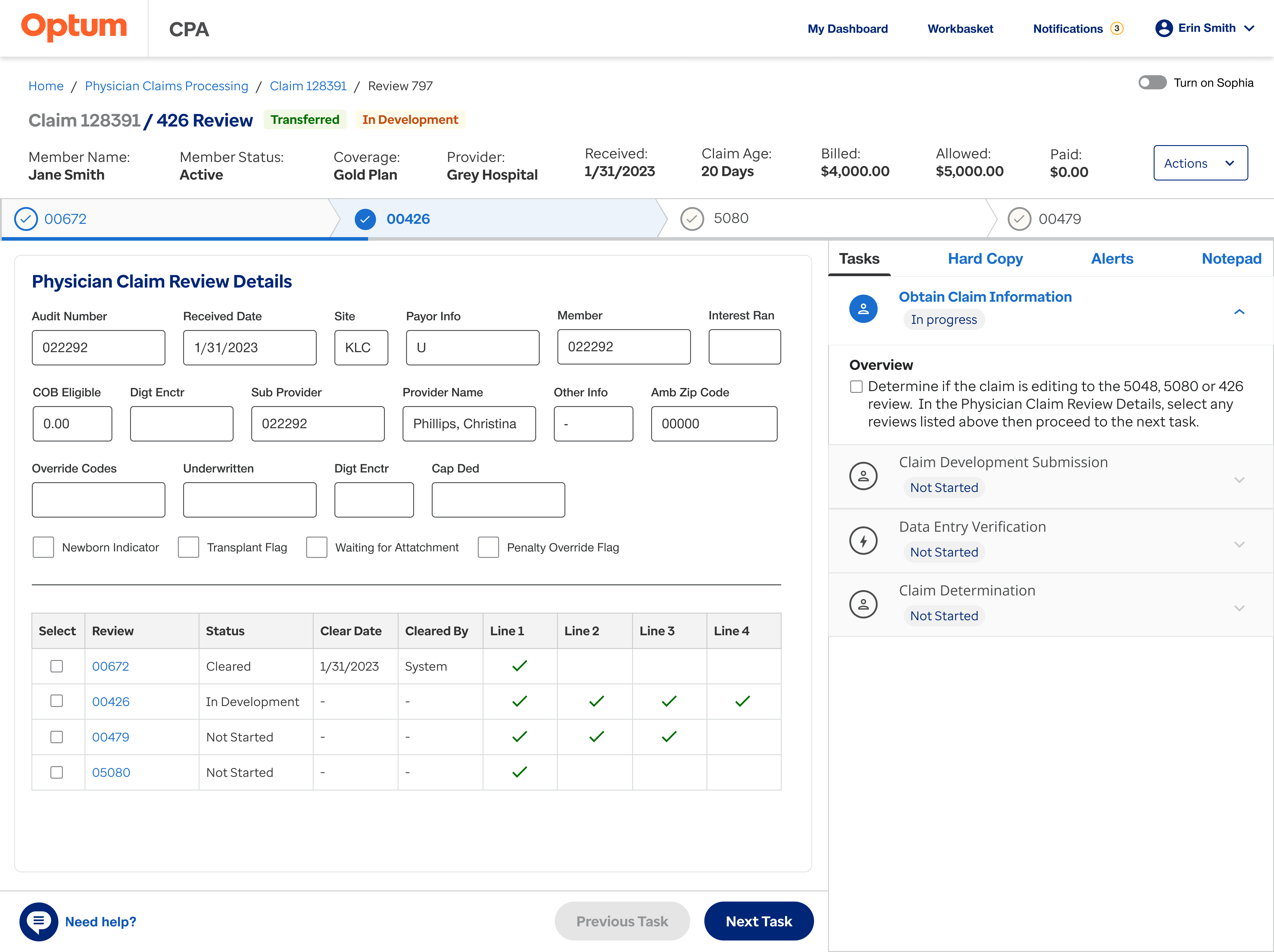
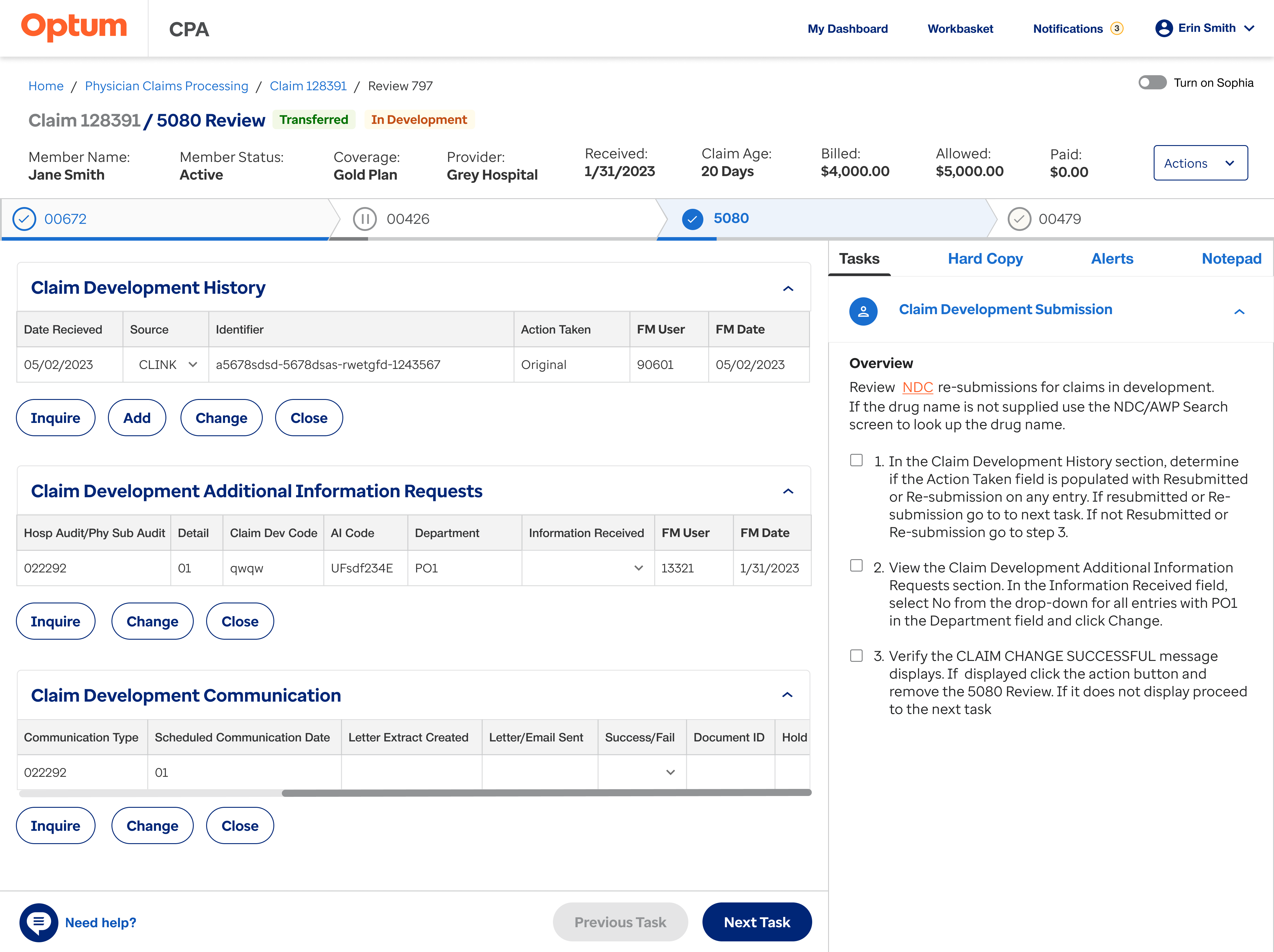
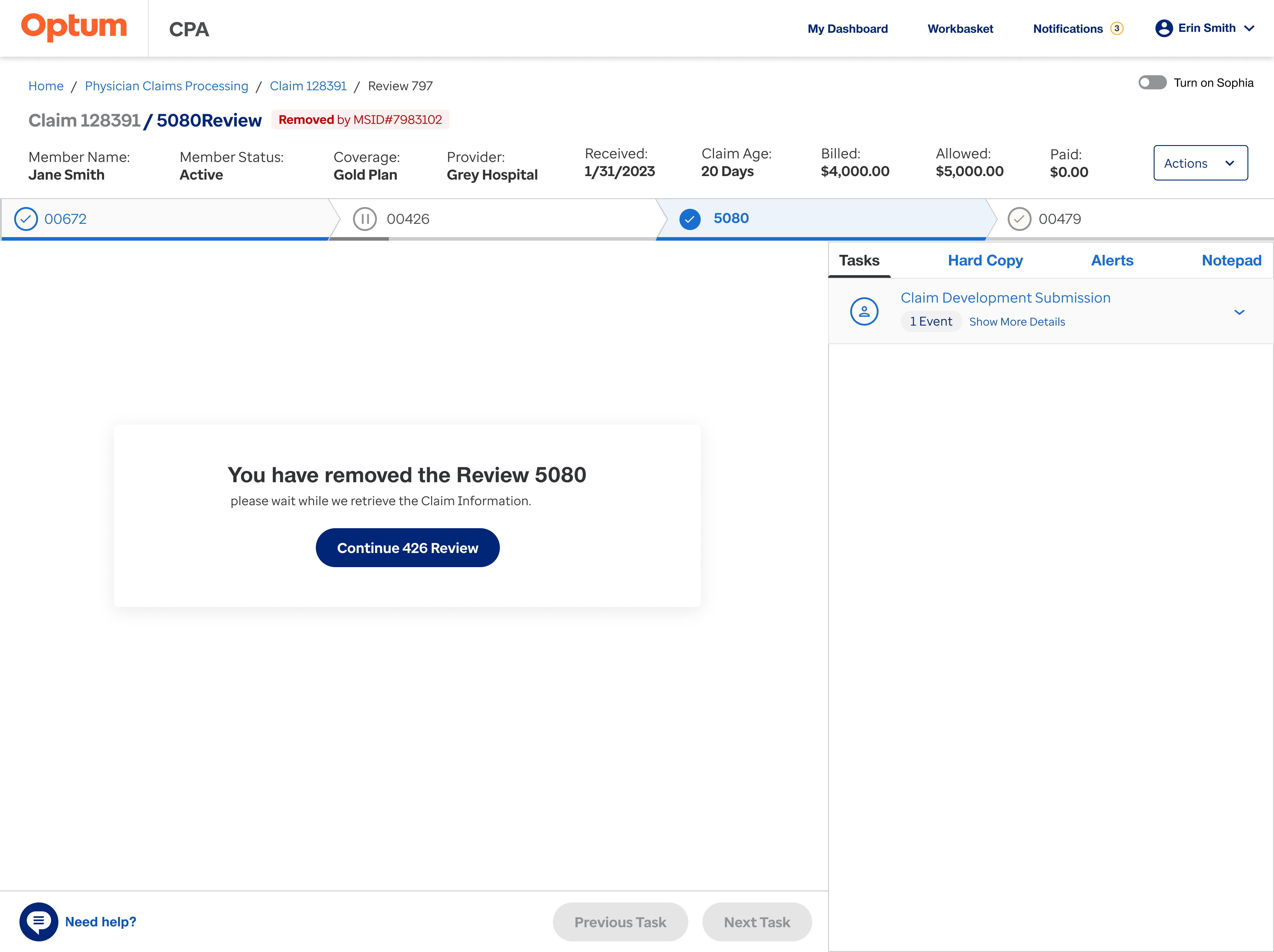
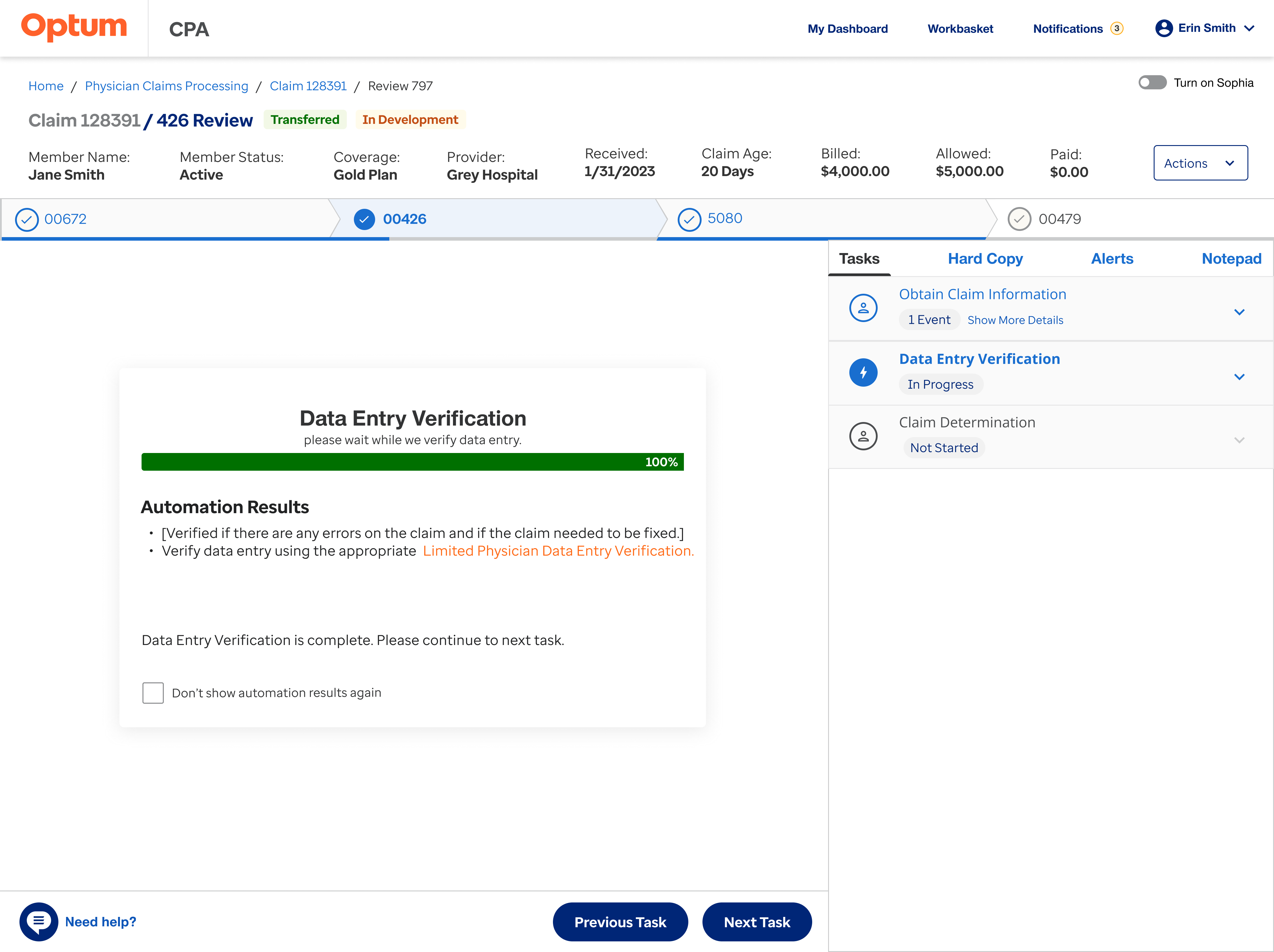
Outdated Interfaces
Processors rely on an old system (CPA) and separate Word documents for claim processing, creating inefficiencies. A unified tool is needed to integrate manual and automated review steps.
Many Processing Resources
Due to complex review instructions and multiple branching processes, processors often manage 10+ open windows per claim, making it difficult to track resources.
Extreme Variation
Claim review process instructions vary by length and complexity based on the type of claim and review needed making standardization challenging.
Limited Effectiveness
Two tools were developed previously to improve the review process, but testing showed they didn’t enhance the experience or scale effectively.
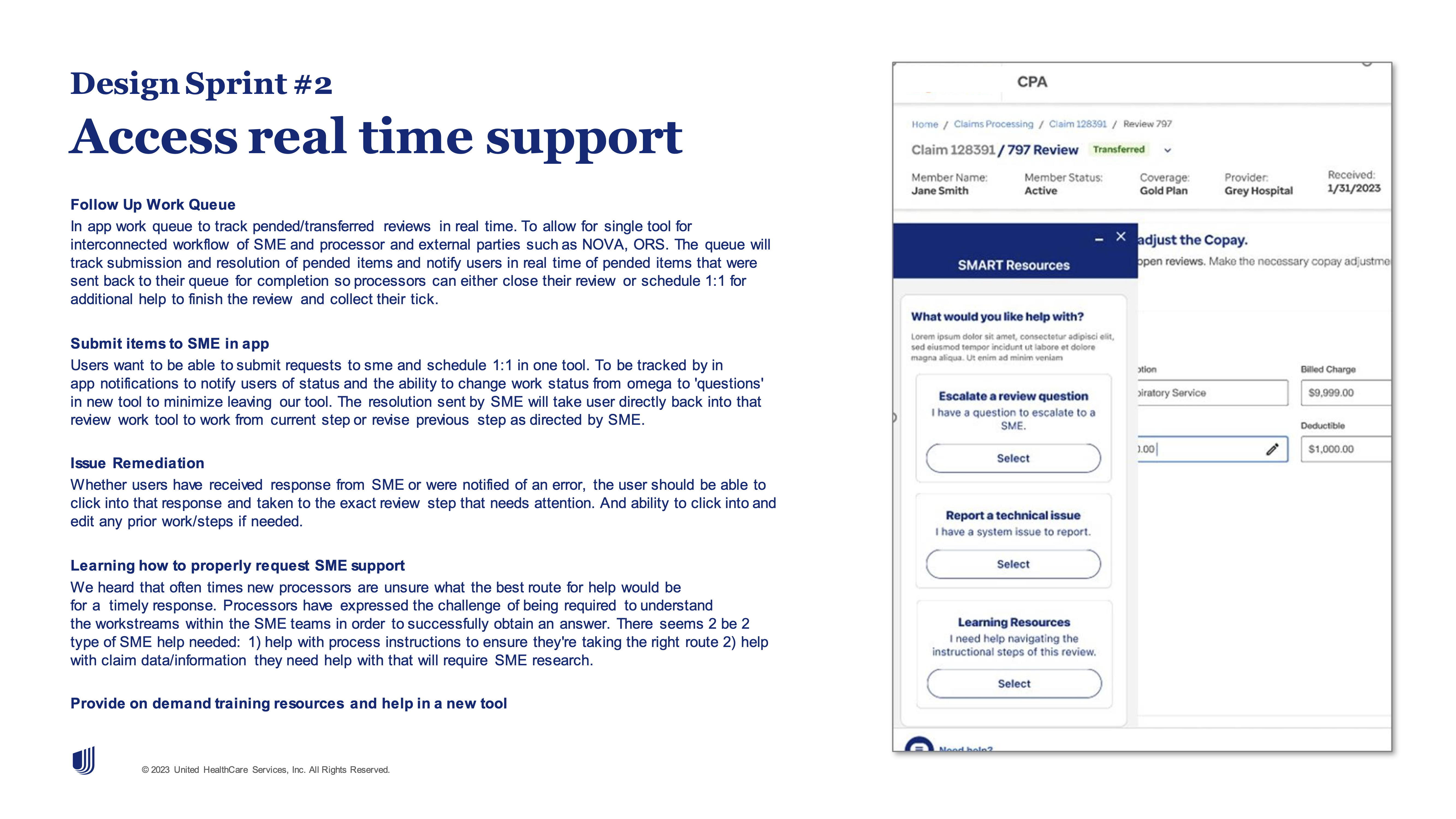
Lack of Real-time Support
Processors need better post-training guidance and resources to handle complex cases efficiently.
High Technical Barrier
Users with limited technical skills struggle navigating the various databases required for claim processing.
Disorganized Training Materials
Resources are fragmented across sectors (e.g., hospital vs. physician) and stored in different locations, making it difficult to access the right information when needed.